Is there a link between care home trading performance and CQC rating?
A question has been raised on whether quality of care comes at a cost - do higher staff costs determine better quality of care? Unsurprisingly, operators that invest heavily within staff training programmes, improve staff retention by creating a good working environment and provide competitive remuneration packages, will be more successful in improving the quality of care.
3 minutes to read
The analysis below comprises a large dataset sample from the financial year 2016/17, which contradicts the above view to an extent.
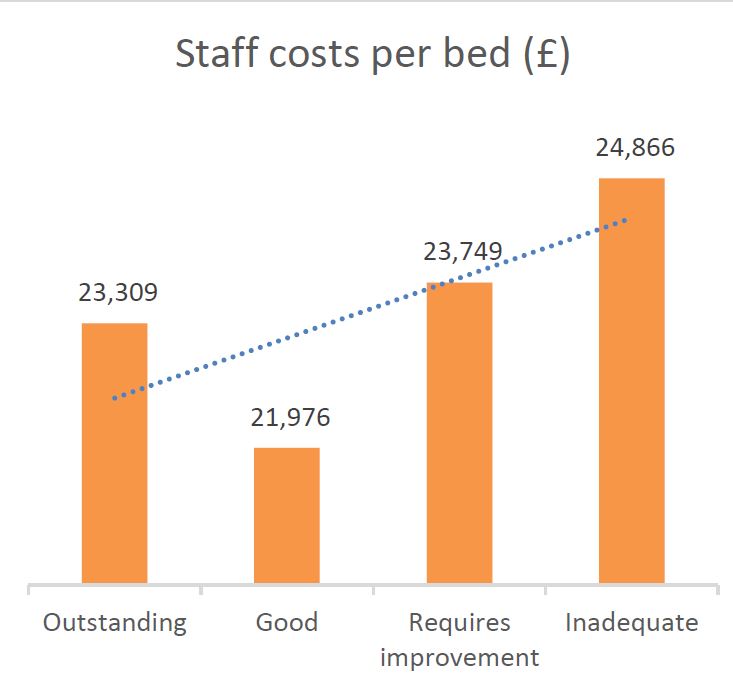
Staffing costs per occupied bed, as shown in Figure 1 are in fact highest for homes rated “inadequate” by CQC, totalling £24,866 per bed when compared with £21,976 per bed for homes rated “good”.
Figure 1
SOURCE: Knight Frank Research
Staff costs are high for homes rated “requires improvement” and “inadequate”, due to high staff turnover and a shortfall of nursing staff, subsequently increasing agency costs. Homes in these categories will typically lack good leadership and a good working environment which demotivates staff leading to high staff turnover. The recruitment process and staff training costs begin to bite and drive up agency staff costs in order to ensure adequate staffing levels are maintained.
Figure 2 supports this view where 15% of total staff costs are attributed to agency costs in homes rated “inadequate” when compared with 3% for those rated “outstanding”.
Figure 2

SOURCE: Knight Frank Research
Interestingly, homes that pay higher wage rates reflect a higher CQC rating as shown in Figure 3. Homes rated “outstanding” pay nurse rates on average of £15.55/hour and carer rates of £8.34/hour when compared with £14.69/hour and £7.54/hour respectively for homes rated “inadequate”.
By advertising competitive wage rates, operators employ good quality, experienced staff and improve staff retention, which determines continuity of care and subsequently improving the quality of care. This of course is not the only driver, as the right ethos needs to be embedded through the home from the top via the Home Manager to ensure that staff provide care in a caring and compassionate manner.
Figure 3

SOURCE: Knight Frank Research
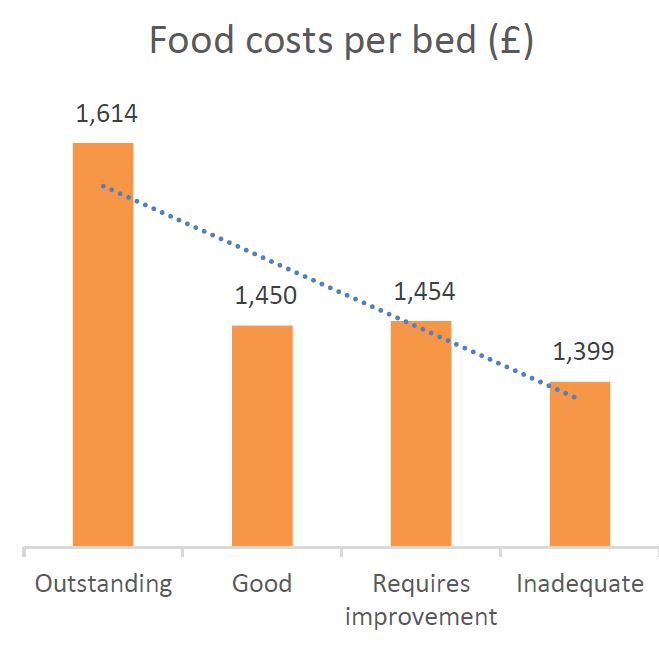
Staff costs are not the only driving factor for quality of care. Figure 4 illustrates food costs per occupied bed by CQC rating, which shows that homes rated “outstanding” spent £1,614 per bed when compared with £1,399 per bed for homes rated “inadequate”.
The higher food costs are driven by operators’ continuous efforts to invest in good quality produce tailored to individual residents, offering choice and a wide variety of fresh fruit, dairy, vegetables, grains and protein, as nutrition for the elderly and specifically for dementia residents is an important area of focus to improve the quality of care.
Figure 4
SOURCE: Knight Frank Research
The other question then to ask is whether a link between quality of care and funding type exists.
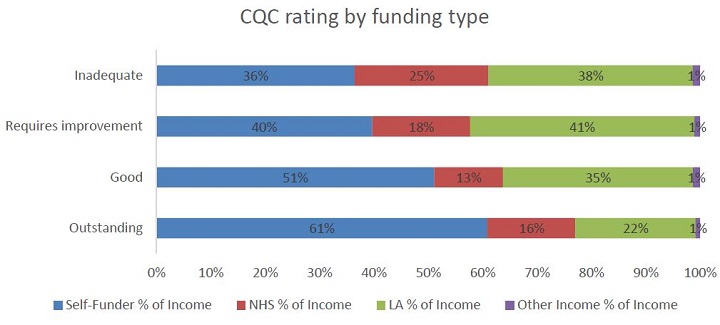
Figure 5 shows the percentage of funding type per CQC rating. It is clear that “outstanding” rated homes are predominately self-funded (61%) and homes rated “requires improvement” and “inadequate” are mainly funded by the local authority (41% and 38% respectively).
“Inadequate” homes also have the highest proportion of NHS funding type. Homes that are mainly privately-funded achieve higher average weekly fees and subsequently make higher profit margins, having more money to invest within their buildings, staff training and technology to improve the level of care provided. This includes electronic care plans and acoustic monitors in order to manage record keeping and staff efficiently.
With the introduction of, and subsequent increase in the National Living Wage, homes funded by the local authority and NHS are feeling the squeeze which limits their capacity to reinvest within their operations.
Figure 5
SOURCE: Knight Frank Research
Going back to the original question, I do not think quality of care is enhanced by employing a higher proportion of staff in the building alone. Staff need to be employed according to individual resident’s care needs and the quality and experience of staff is key – continuity of staff is key!
Figure 6

SOURCE: Knight Frank Research
For more information contact: